How prior authorization works
Prior authorization (also called "preapproval" or "precertification") is what your health insurance may require to approve certain medications or procedures before they begin paying for your treatment. It’s essentially your healthcare provider providing documentation that the medication or care they prescribed is medically necessary.
Typically 5 days for Nurtec ODT
Timing may vary. If you don't hear about the status of your prior authorization
request within 5 days, follow up with your healthcare provider.
What to discuss with your healthcare provider
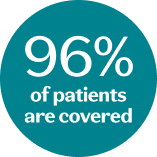
96% of patients with commercial insurance are covered for Nurtec ODT, and in most cases, your healthcare provider can handle the entire prior authorization process.
However, the top reason prior authorizations for Nurtec ODT are rejected is because they are missing information, so it's important to make sure your healthcare provider has all of the below:
https://main--nurteccom--pfizer.hlx.page/global/fragments/healthcare-checks
Learn more about what to share with your healthcare provider.
Call one of our live specialists for personalized support
A Pfizer Migraine Patient Access Coordinator can help answer questions about insurance coverage, cost/savings, or prior authorization for your Nurtec ODT therapy.
Call our team now: 1-866-222-4183 |
Monday–Friday, 8:00 AM-8:00 PM ET
Your go-to spot for additional information, resources, and personalized assistance with insurance.
What happens if my prior authorization request is denied?
You still have options. Sometimes even simple clerical errors can affect a request. So, the first step is to find out why. Your healthcare provider should be able to help. If you think the denial was not justified, you and your provider may choose to appeal.
OTHER THINGS YOU CAN DO:
Contact your healthcare provider to review your insurance requirements to ensure you meet them.
Provide your healthcare provider with any additional information that may be needed to resubmit your prior authorization.
Nurtec ODT offers a $0 copay card
You don’t have to delay starting your treatment. If you are eligible, you can get your first prescription at no cost* even if your prior authorization is still being processed by using the copay card at your local pharmacy.
Sign up for your copay card to pay as little as $0*
Eligible commercially insured patients can download their copay card to get Nurtec ODT for less.

*Eligible commercially insured patients can, for one time only, access Nurtec ODT at no cost while benefits are being verified for one prescription fill, with a maximum of 16 tablets total. Insurance coverage must be approved by the payor for patients to continue receiving Nurtec ODT with no out-of-pocket cost. No membership fees. Only available for commercially insured patients. This is not health insurance. Maximum annual benefit of $7,000 applies. The full terms and conditions can be accessed at nurtec.com/terms-and-conditions.

